
7 Ways to Improve an Already Effective Treatment for Stimulant Use Disorder
The opioid epidemic has been one of the most pressing and challenging issues that the U.S. has faced in recent decades, with countless lives lost to this devastating crisis. Now, stimulant-related overdoses are among the next big drug-related concerns, with recent studies showing that the mortality rate linked to stimulant use in the U.S. has […]

Economic Evaluations of Establishing Opioid Overdose Prevention Centers in 12 North American Cities: A Systematic Review
In this systematic literature review published in Value in Health, CHERISH Research Affiliates Czarina Behrends and Ahmed Bayoumi, CHERISH staff members Jared Leff, Jazmine Li, and Erminia Fardone, CHERISH investigators Kathryn McCollister, Sean M. Murphy, and Bruce Schackman, and former NIDA summer intern, Weston Lowry, analyzed 16 studies that summarized and identified gaps of economic […]

New Study Reveals Preventable-Suicide Risk Profiles
Individuals with physical health concerns made up the largest and fastest growing of five subgroups of individuals who died by suicide n the United States over roughly twenty years, according to an analysis led by Weill Cornell Medicine in collaboration with Columbia University, UC Berkeley School of Public Health, the University of Hong Kong and […]

Surgeons Are Closer to Predicting Which Patients Need Post-Surgery Opioids—and Which Ones Don’t
Opioids are routinely prescribed to patients after a surgery—whether they use them or not. A new study, led by LDI Senior Fellow Anish Agarwal will help tailor prescribing so patients get the right amount of opioid medications; not too little and not too much. Unused opioids are a particular problem. Opioid misuse can start when extra tablets […]

Chart of the Day: Rise in Patients with Opioid Use Disorder Leaving Hospital Prematurely
LDI Senior and Associate Fellows Ashish Thakrar, Margaret (Maggie) Lowenstein, Ryan Greysen, and M. Kit Delgado found that more people with opioid use disorder are leaving the hospital prematurely (or before medically advised), compared to marginal increases for individuals admitted for other reasons. In the study, “Trends in Before Medically Advised Discharges for Patients with Opioid Use Disorder, 2016-2020,” […]
Back in Person and Taking a Bite of the Big Apple
Over the course of three days, from October 18-20, 2023, the annual Addiction Health Services Research (AHSR) Conference brought over 300 attendees to Roosevelt Island in New York City to share new addiction research findings, learn about the field through pre-conference workshops, develop collaborative relationships, and support early-career and under-represented investigators. “I am so proud […]

Sharing Your Research for Maximum Impact
In today’s digital and media landscape, there are several ways to disseminate your health economics research after its publication. From our experience, writing social media, news posts, and policy briefs has allowed us to convey study findings from different angles, reach new audiences, and inform key decision makers. As you are preparing your next journal […]

Stigma and Sluggish Bureaucracy Block Treatment for Stimulant Use Disorder
So, imagine there’s a runaway epidemic of overdose deaths that involve non-opioid drugs and that we’ve had an evidence-based therapy for this unique addiction for the last forty years—but for reasons largely grounded in legislators’ and the public’s visceral disdain for people who use substances, we have refused to nationally recognize or widely implement this […]

Incentivizing Recovery: Payment, Policy, and Implementation of Contingency Management
On January 19th, 2024, CHERISH and the University of Pennsylvania’s Leonard Davis Institute of Health Economics (LDI), co-hosted a virtual convening titled Incentivizing Recovery: Payment, Policy, and Implementation of Contingency Management. Contingency management is a proven and promising treatment for specific substance use disorders, especially stimulant use disorder. However, significant gaps in knowledge regarding the […]
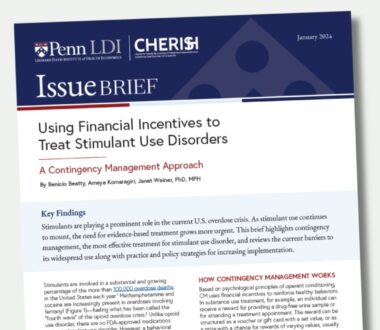
Using Financial Incentives to Treat Stimulant Use Disorders
Stimulants are involved in a substantial and growing percentage of the more than 100,000 overdose deaths in the United States each year. Methamphetamine and cocaine are increasingly present in overdoses involving fentanyl—fueling what has been called the “fourth wave” of the opioid overdose crisis. Unlike opioid use disorder, there are no FDA-approved medications to treat […]

Many State Medicaid Programs Still Require Prior Authorization for Buprenorphine Treatment for Opioid Use Disorder
The opioid epidemic has been an ongoing public health crisis in the United States, claiming countless lives and devastating communities. Buprenorphine, a highly effective medication for the treatment of opioid use disorders, holds the potential to save lives. However, a significant hurdle exists in the form of prior authorization requirements, which are associated with lower access to […]

LDI Experts Analyze the New U.S. Plan to Target Xylazine-Laced Fentanyl
The lethal mixture of xylazine and fentanyl, also known as Tranq dope, may sound unfamiliar to many, but its impact is harming people who use drugs nationwide. Xylazine, approved by the U.S. Food and Drug Administration for veterinary use as a sedative, has become a major component in the illicit drug trade. When consumed by humans, xylazine causes […]
Engage with CHERISH
Submit a Consultation Request or Contact Us to learn more about how CHERISH can support your research or policy goals.