Will Eliminating Waiver Requirements Improve Access to Buprenorphine for Treating Opioid Use Disorder? Evidence From Increasing the Patient Treatment Cap

The Drug Addiction Treatment Act of 2000 (DATA 2000) permits qualified physicians to obtain a waiver to treat patients with opioid use disorder (OUD) with buprenorphine in office-based practices. In 2016, 47% of all US counties and 72% of rural counties lacked a buprenorphine waivered physician. That year, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing privileges to nurse practitioners and physician assistants who meet training requirements. Obtaining the waiver requires 8 hours of training for physicians and 24 hours of training for nurse practitioners and physician assistants. These professionals can only prescribe buprenorphine to a maximum of 30 patients during the first year after obtaining a waiver, and in the subsequent years they can apply to treat more patients.
Although there has been growth in the number of waivered providers, less than five percent of practicing physicians, nurse practitioners, and physician assistants are waivered to prescribe buprenorphine. Some believe that that the waiver regulations pose an undue burden on providers. They argue that removing the waiver would increase the number of providers prescribing buprenorphine and recommend that this training should be incorporated into medical school training or waivers should be provided at a system level instead.
Others point out additional barriers that contribute to buprenorphine underutilization including lack of institutional and clinician peer support, poor care coordination and siloed care that is reinforced by burdensome reimbursement models. They argue that training is necessary and could be modified to reduce the burden to providers by adjusting the number of requisite hours, addressing stigma, making more training options available for free, and creating apprentice-based training models. They also argue for removing or expanding patient limits for addiction medicine or addiction psychiatry specialists.
Contributing evidence to this debate, recent studies have examined the impact of removing waiver prescription limits. In 2016, the Department of Health and Human Services increased the maximum allowable number of buprenorphine patients per waivered physician from 100 to 275. Two research teams examined the effect of this increased patient cap on buprenorphine treatment availability using data from the US Drug Enforcement Agency.
Lee-Kai Lin, Kosali Simon, Alex Hollingsworth and CHERISH Research Affiliate Brendan Saloner compared the total amount of buprenorphine dispensed per capita in each 3-digit zip code in 2015 (before the policy change) and 2017 (after the policy change). Their findings suggest that the greater the number of waivered physicians, the more buprenorphine is available per capita. The study estimates that adding one more waivered physician increases access for 3.6 patients in the 3-digit zip code, and that the amount of access improvement is greater with higher patient limits; physicians with a 100-patient waiver increase access for 8.71 patients, and physicians with a 275-patient waiver would access for 44.09 patients. They did not identify a statistically significant effect for nurse practitioners and physician assistants, who were limited to 30 patients in the time period they studied. The authors interpret their findings as suggesting that increasing the number of 275-patient providers would be more effective for expanding buprenorphine treatment than increasing the number of physicians with 30-patient waivers.
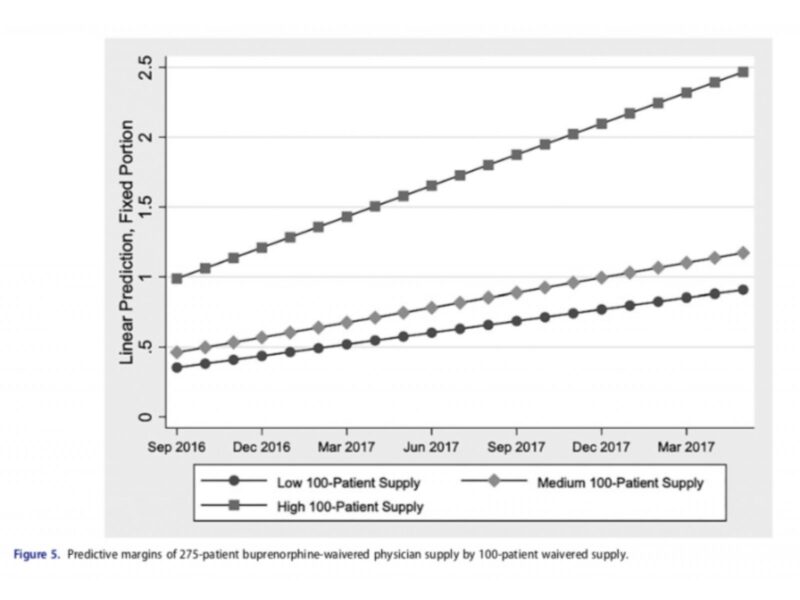
Hannah Knudsen, Lewei (Allison) Lin and Michelle Lofwall examined the number of waivered physicians in each state over the 21 months following the policy change from September 2016 to May 2018. During this period, the number of physicians with a 275-patient waiver increased from 153 (mean 0.07 per 100,000 state residents) to 4,009 (mean 1.42 per 100,000 state residents), while the number of physicians with a 100-patient waiver fell from 10,256 (mean 3.62 per 100,000 state residents) to 8,643 (mean 3.04 per 100,000 state residents). In multivariate analysis, states in New England and states with a greater pre-existing supply of 100-patient waiver physicians had higher rates of uptake of the 275-patient waiver over the 21 months and states with higher supply of licensed opioid treatment programs per capita had lower rates of uptake of the 275-patient waiver. Rates of uptake were not associated with state-level measures of opioid overdose mortality and unmet illicit drug treatment need. The authors conclude that uneven patterns of growth uptake of the 275-patient waiver pose a challenge to efforts to increase buprenorphine treatment availability.