A Cost-Effectiveness of Implementation Facilitation to Promote Emergency Department–Initiated Buprenorphine for Opioid Use Disorder
Implementation facilitation shows promise in promoting buprenorphine treatment in the emergency department.

In the last eight years, emergency departments (EDs) have seen an influx of visits related to opioid use disorder (OUD).
For the same reason, researchers have been citing EDs to be a critical setting and reachable moment for initiating OUD medications, the gold standard of care.
Buprenorphine is advantageous as a low-barrier OUD treatment compared to methadone and naltrexone, the other FDA-approved OUD medications. Buprenorphine is typically preferred by patients over naltrexone, which requires full detoxification from opioids before initiation, and can easily be prescribed in the ED unlike methadone, which requires prescribers to be affiliated with a certified opioid treatment program. Despite evidence of buprenorphine’s effectiveness in the ED, with regard to improving the likelihood of treatment initiation and subsequent linkage to community-based care, ED clinicians have reported barriers to introducing buprenorphine to patients.
Lead author and CHERISH Research Affiliate Thanh Lu examined the economic value of using implementation facilitation (IF) to enhance the readiness of clinicians and staff for incorporating a buprenorphine and treatment linkage program in an ED. Co-authors of the study include CHERISH Research Affiliate Ali Jalali, senior author and CHERISH Methodology Core Co-director Sean M. Murphy, and colleagues from Yale’s Schools of Medicine and Public Health.

Thanh Lu, PhD
CHERISH Research Affiliate, RTI International
Grand Rounds vs Implementation Facilitation
The researchers led a cost-effectiveness analysis alongside Project ED Health, a clinical trial that took place at four academic emergency rooms and enrolled 756 patients with moderate-to-severe OUD. The IF intervention was compared to a standard grand rounds strategy, which engaged clinicians in a 60-minute presentation about ED-initiated buprenorphine, safe prescribing, overdose education, and naloxone distribution. The IF involved identifying relevant characteristics and barriers to the ED, finding a “local champion” for the ED-buprenorphine program, and connecting with community-based treatment programs to facilitate referrals, provider education, focus groups, and other meetings to tailor the program to each ED site. The economic evaluation was conducted from the healthcare-sector perspective, accounting for all direct medical costs incurred on behalf of patients. Key measures of effectiveness included quality-adjusted life years (QALYs), opioid-free years (OfYs), and engagement in community-based OUD care at 30 days after the intervention.
The Value of Implementation Facilitation
From the perspective of the healthcare-sector, IF has a moderate-to-high likelihood of being a cost-effective strategy to initiate buprenorphine in an ED setting.
The findings were in favor of IF:
- IF, compared to a standard educational strategy, was more effective with regard to QALYs and OfYs gained, and likelihood of engagement in community-based OUD care. On average, participants in the IF intervention experienced a 6 percentage-point increase in the probability of treatment engagement within 30 days, an additional 51 days of perfect health, and 29 days free from opioids over one year.
- The total cost of IF to the healthcare sector was less—though not significantly different—than the standard educational strategy.
- IF’s probability of cost-effectiveness was 74%-75% at the recommended cost/QALY threshold range of $100,000-200,000; it reached the same level of confidence at $25,000 per OfY and $38,000 per treatment engagement.
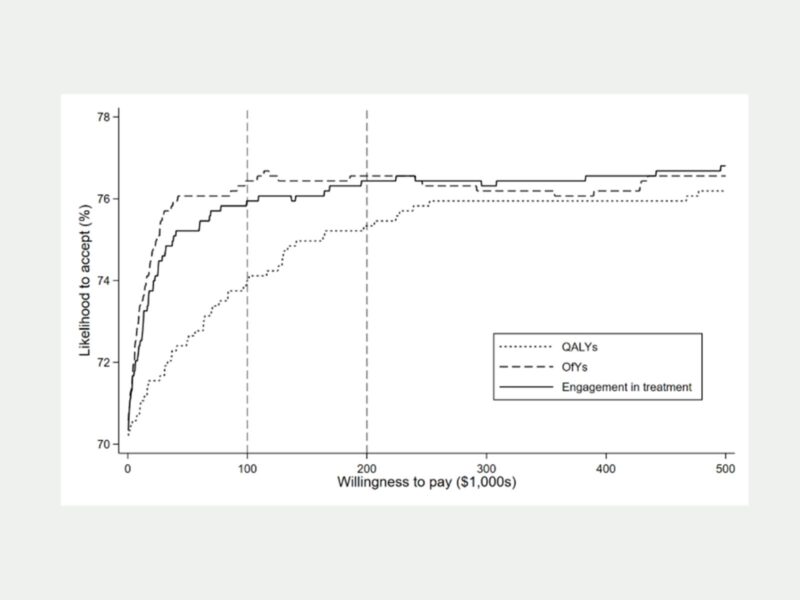
On average, participants in the IF intervention experienced significantly higher levels of effectiveness than those in the standard education strategy, without incurring higher costs. The probability that IF would be considered cost-effective reached a maximum of 75% within the recommended value-threshold range of $100,000 – $200,000 per QALY gained. Researchers emphasize that start-up costs, which are not included in cost-effectiveness analyses, will be an important consideration for facilities interested in using IF to create a similar ED-buprenorphine program; however, upon reaching a steady-state, the program demonstrates a reasonably strong economic value.
The study, “Cost-Effectiveness of Implementation Facilitation to Promote Emergency Department-Initiated Buprenorphine for Opioid Use Disorder,” was published in Annals of Emergency Medicine on November 20, 2024.