Characterizing Initiation, Use, and Discontinuation of Extended-Release Buprenorphine in a Nationally Representative United States Commercially Insured Cohort
Medications for opioid use disorder (MOUD) are evidence-based treatments that help people reduce or stop using opioids. However, high discontinuation rates of MOUD pose a barrier to reducing opioid-related overdoses. Extended-release buprenorphine (XR-BUP) is a relatively new MOUD, approved in late 2017, that has the potential to increase retention because of its monthly dosing schedule. Currently, there is a lack of data comparing XR-BUP initiation, use, and discontinuation to other medications for OUD in real-world settings.
To determine if XR-BUP reduces rates of discontinuation, researchers affiliated with the Center for Health Economics of Treatment Interventions for Substance Use Disorder, HCV, and HIV (CHERISH), Boston Medical Center, and Boston University School of Public Health and School of Medicine, led a study to measure discontinuation rates among a national cohort of 14, 358 individuals who had employer-sponsored insurance and started one of four medications for OUD in 2018: extended-release formulations of buprenorphine (XR-BUP) and naltrexone (XR-NTX), both with monthly dosing, and oral formulations of buprenorphine (mucosal buprenorphine, M-BUP) and methadone, both with daily dosing.
CHERISH-affiliated authors found that discontinuation, defined by a gap of 14-or-more days in medication coverage, was common across all four medications for opioid use disorder.
The authors found that discontinuation, defined by a gap of 14-or-more days in medication coverage, was common across all four MOUD. Specifically, three months after initiation, 50% of XR-BUP, 64% of XR-NTX, 34% of M-BUP, and 58% of methadone initiators had discontinued treatment. Additionally, they found that those who discontinued treatment by three months were more likely under 30 years of age, managing multiple comorbidities, and diagnosed with concurrent substance use.
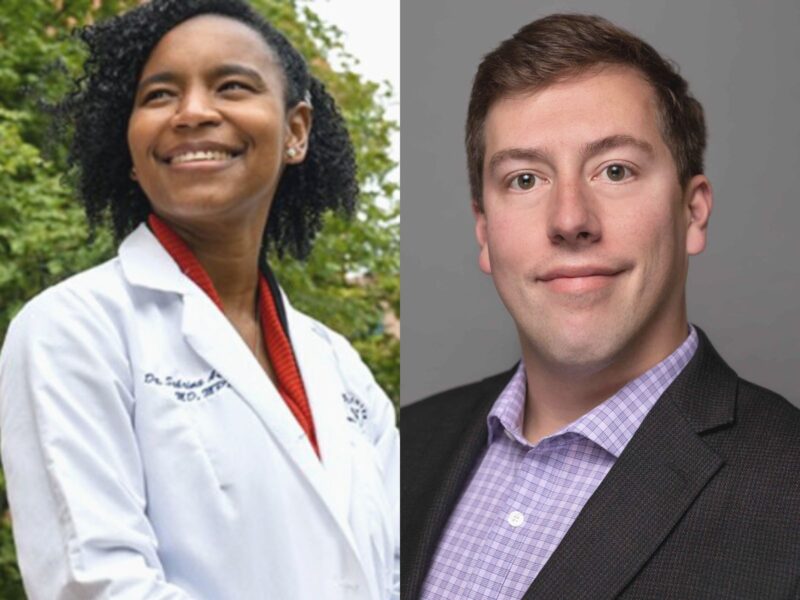
CHERISH Research Affiliate Sabrina Assoumou, an infectious diseases physician at Boston Medical Center who is the study’s senior author, was hopeful that XR-BUP would be a promising solution to improving retention. “We thought that the critical component was going to be an injectable formulation, but what the data are telling us is that it’s not going to be that easy,” says Assoumou, “and we’re really going to have to work to support our patients during this critical time to help them stay on track.”
Observing that XR-BUP alone was not associated with significantly better retention at three months, the authors suggest that health care providers can improve retention by:
- Prioritizing patient needs and preferences when choosing treatment
- Providing support during the first month of treatment, when discontinuation rates are highest, and flexibility for patients to switch medications
- Integrating MOUD with behavioral and residential care for individuals with comorbidities
“We always want more medication choice, not less, since every patient is unique,” says CHERISH investigator and study lead author Jake R. Morgan, a research assistant professor at Boston University School of Public Health. “This study adds context to opioid use disorder as a chronic, relapsing disease. Providers should expect that discontinuation is often a part of the treatment process, and consider what sort of clinical approach they will take when it occurs.”
The authors propose several areas for further research and exploration to continue investigating the high discontinuation rates and carefully parse out the individual effects of XR-BUP compared to other MOUD:
- Understand aspects of patient-centered decision-making that could interfere with retention, such as cost barriers, dose adjustments, co-prescribing with M-BUP, or using XR-BUP to transition between MOUD
- Determine why individuals under 30 are more likely to use injectable MOUD and discontinue treatment
- Determine why individuals with more competing health priorities are more likely to use injectable MOUD
- Explore the disconnect between qualitative research that identify injectable medications, like XR-BUP, as favorable for its convenience, and real-world data that show high discontinuation rates for injectable MOUD
Authors of the article include CHERISH investigator Drs. Jake R Morgan, Alexander Walley, Sean Murphy, and Benjamin Linas; CHERISH Research Affiliate, Drs. Joshua Barocas and Sabrina Assoumou; and Drs. Avik Chatterjee and Scott Hadland of Boston Medical Center and Boston University School of Medicine.
Read the full paper in Drug and Alcohol Dependence.