Insurance Instability for Patients with Opioid Use Disorder in the Year After Diagnosis
Researchers explored the insurance instability among adults diagnosed with OUD in Massachusetts in a new longitudinal cohort study.
Access to health insurance is crucial to gaining the necessary diagnostic and therapeutic services to achieve and maintain good health.
Insurance is especially necessary to access medications for opioid use disorder (MOUD) as the cost of MOUD can be a barrier to staying in treatment. If insurance coverage is disrupted, MOUD treatment may be more likely to be discontinued, which can often lead to poor health outcomes including higher mortality. In this new study featuring CHERISH investigator Jake R. Morgan, researchers investigated insurance instability in patients with newly diagnosed opioid use disorder to learn more about who is most affected by insurance disruptions.

Jake R. Morgan
CHERISH investigator at the Boston University School of Public Health
Using data from the Massachusetts Public Health Data Warehouse, the team of researchers conducted a retrospective cohort study to identify the incidence of insurance transitions within 1 year of diagnosis. They defined an incidence as any transition away from their original insurance at the time of diagnosis into another insurance or a lack of insurance during their follow-up visits. As there are known inequities in MOUD access, researchers estimated the probability of insurance transition across sociodemographic groups including race and ethnicity.
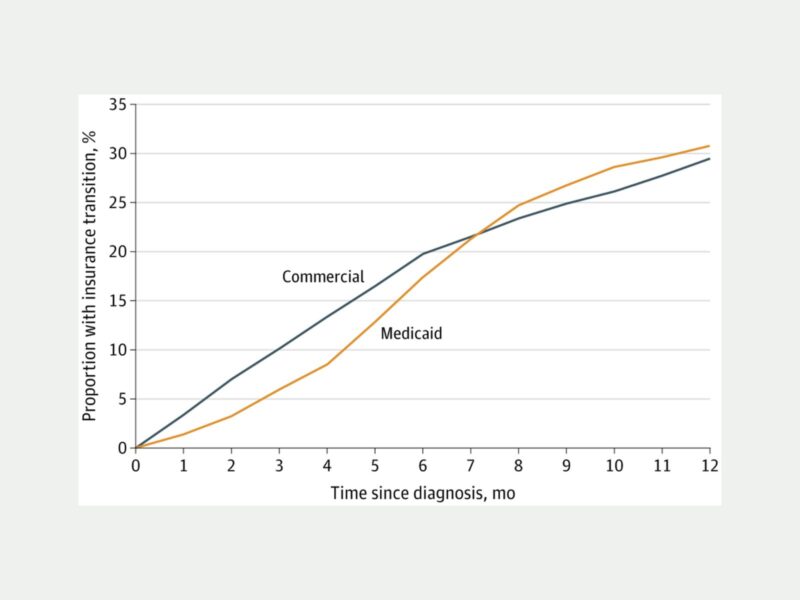
Researchers found that nearly 1 in 3 individuals diagnosed with OUD experienced an insurance transition within 1 year of their diagnosis. The rates differed by insurance type, age, race, and ethnicity.
Key Findings
- 3 out of 10 people with OUD experienced an insurance transition within 1 year of their diagnosis.
- Younger individuals with OUD, regardless of insurance type, were most likely to experience insurance transition. Those between ages 26 and 35 and insured by commercial insurance had an especially high risk of transition.
- Black non-Hispanic individuals with OUD and insured by commercial insurance had the highest risk of insurance transition followed by Hispanic individuals insured by commercial insurance. These differences were less prominent among individuals covered by Medicaid.
- Individuals insured by Medicaid were more likely to initiate MOUD at the time of diagnosis compared to those covered by commercial insurance. The initiation of MOUD in individuals insured by Medicaid was associated with nearly a 6% reduction in insurance transition rates.
This longitudinal study is one of the first to assess the issue of insurance instability among individuals who were newly diagnosed with OUD. Previous studies and policies have primarily focused on increasing insurance enrollment to improve overall well-being. However, as this study demonstrates, many individuals with OUD experience an insurance transition within one year of OUD diagnosis. These individuals face a higher risk of treatment disruption.
Sensitivity analyses indicated that individuals with commercial insurance had higher rates of insurance transitions than individuals with Medicaid. This difference could imply difficulties in maintaining employment because individuals seeking treatment may face stigma from their employers or drug use may interfere with their ability to perform their job duties. As insurance instability may hinder coverage of MOUD, the authors suggest that future research directions look into the relationship between changes in treatment outcomes and insurance transitions for patients with OUD.
Read the full study published in JAMA Health Forum.