The announcement is a product of the work of the Substance Use Disorder Treatment Task Force, led by Gary Mendell, CEO of Shatterproof, and Thomas McLellan, founder and chairman of Treatment Research Institute. The Task Force, launched in April 2017, included members representing payers, government agencies, advocacy, and academia. LDI Executive Director Dan Polsky serves on the Task Force Steering Committee.
“This is an important step in closing the gaps in treatment,” Polsky said. “Bringing payers to the table is essential if we want to improve access to care and the quality of that care for people with addictions.”
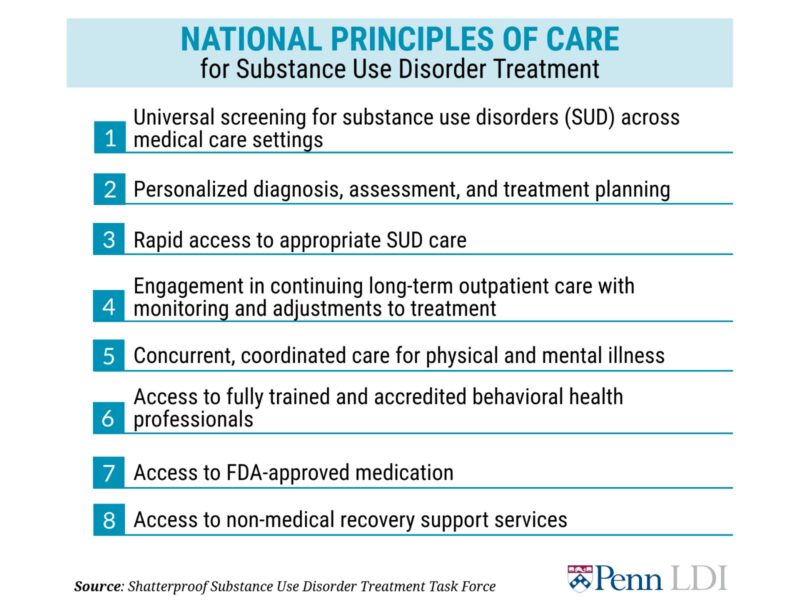
Insurers in yesterday’s announcement include: Aetna, AmeriHealth Caritas Family of Companies, Anthem, Inc., Beacon Health Options, Blue Cross Blue Shield of Massachusetts, CareSource, Centene Corporation, Cigna, Envolve Health, Horizon Blue Cross Blue Shield of New Jersey, Magellan Health, and United Health Group. These organizations have committed to identifying, promoting, and rewarding substance use disorder treatment that aligns with the National Principles of Care.
Polsky pointed out that the principles were based on evidence and recommendations included in the Surgeon General’s Report on Alcohol, Drugs, and Health and consistent with previous work on the cost-effectiveness of opioid use disorder treatments. He also noted that the Task Force itself exemplifies how researchers, policymakers, and other stakeholders can work together define and align their goals, a subject of a recent conference sponsored by LDI and the Center for Health Economics of Treatment Interventions for Substance Use Disorders, HCV, and HIV (CHERISH).
Last year, more than 64,000 people in the United States died of a drug overdose, a figure that has nearly doubled over the past decade. With the opioid epidemic and substance use disorders gripping the nation, payers are a crucial component and partner in stemming the carnage.