Optimizing HIV Prevention in Six US Cities: An Economic Model
In 2019, the United States launched the effort to End the HIV Epidemic by reducing new infections by 75% within 5 years and by 90% within 10 years. This national strategy comes with some new funding for the Centers of Disease Control and Prevention (CDC), the Health Resources and Services Administration (HRSA), and the Ryan White HIV/AIDS Program focused on 48 affected counties, Washington DC, San Juan Puurto Rico, and 7 southern states. To help cities spend HIV funds wisely, CHERISH Research Affiliate Bohdan Nosyk and colleagues developed an economic model that identified the combinations of evidence-based interventions with the greatest likelihood of reducing HIV transmission over 10 years in six cities. The study, published in Lancet HIV, examined the level of scale-up and implementation of 16 evidence-based strategies required to address these local micro-epidemics, and ultimately reduce HIV-related disparities.
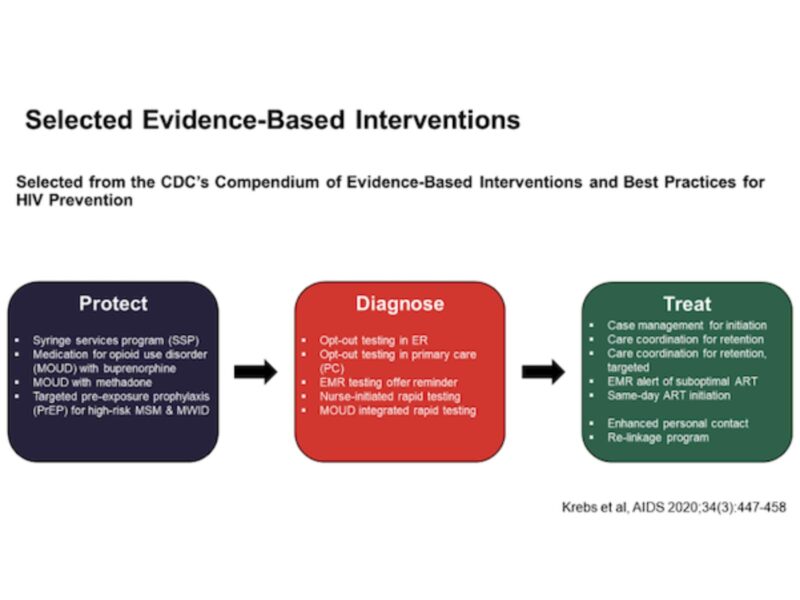
Nosyk and colleagues used a dynamic model that reflected HIV micro-epidemics in Atlanta, Baltimore, Los Angeles, Miami, New York City, and Seattle, which together have almost one quarter of all people living with HIV in the US. Data for the model were largely city-specific, producing results that reflected local economic resources, HIV transmission patterns, and service levels that would affect cost-effectiveness of different interventions (Figure 1). These interventions were modeled at both conventional and optimal levels of scale-up and implementation. They then compared the costs and effects of these interventions on HIV prevention to the status quo over a 10-year time horizon.
Depending on the city, intervention combinations included 9-13 strategies that produced the greatest health benefits while remaining cost-effective. Access to medication for opioid use disorder (MOUD), electronic medical record testing offer reminders, nurse-initiated rapid HIV testing, rapid testing in MOUD and ART engagement or re-engagement interventions were included in intervention packages across all cities; opt-out testing in the emergency department and primary care setting, and non-targeted care coordination to improve ART were not included in any city. These results give local policymakers insight into the best use for that additional dollar of HIV spending; for example, expansion of syringe service programs to prevent HIV was only recommended for cities that did not have high levels of existing syringe-exchange services, including Atlanta, Los Angeles, and Miami. Expansion of PrEP for high-risk men who have sex with men was only included for Atlanta, Baltimore, Los Angeles, and Miami. Expanded PrEP became an optimal strategy elsewhere if the medications were donated by the manufacturer.
Optimal strategy combinations were cost saving in Atlanta, Baltimore, and Miami, meaning the health care gains outweighed the costs of implementing and delivering the health services at a conventional level. These strategies were cost-effective in the remaining cities at a threshold of $100,000 per quality-adjusted life year (QALY).
But even the optimal strategy implemented at conventional levels would not achieve national HIV goals: the model suggests that HIV incidence would decrease by about 38% by 2030, which is less than half the national goal. Significant additional investment and unprecedented scale-up of service delivery would be required to meet national goals. In an invited commentary, Drs. Brooke Nichols and Stephen Kissler point out that these strategies still require a large initial investment in order to achieve long-term benefits, and emphasize the need for similar modeling in rural settings that may face additional barriers to service access.
In March 2020, Dr. Nosyk was awarded supplemental funding from the National Institute on Drug Abuse (NIDA) that will support a collaboration with CHERISH Dissemination & Policy Core leaders Dr. Zachary Meisel and Dr. Janet Weiner at the University of Pennsylvania’s Leonard Davis Institute of Health Economics. Together, they will communicate the findings to local decision makers in each city and identify opportunities to support local decision making. “In our discussions with stakeholders and policymakers, they have expressed the need for data that addresses local circumstances. This supplemental study provides us with the opportunity have those meaningful and productive conversations,” said Janet Weiner.