Overdose and Re-hospitalization Rates Following Endocarditis Are Lower for Patients Receiving Medications for Opioid Use Disorder
The proportion of hospital admissions for endocarditis attributable to injection drug use increased from 7% in 2000 to 12% in 2013. Endocarditis is an infection in the lining of the heart chambers and valves that can be contracted through shared injection equipment. Rates of endocarditis are disproportionately affecting young people who inject drugs (PWID), which has long term health consequences and affects future healthcare utilization. Endocarditis treatment often includes valve replacement and a lengthy course of antibiotics, which lead to costly long-term hospitalizations and may lead to prosthetic valve infections that require re-treatment. Among those who have been treated for endocarditis, estimates of reinfection range from 13% to 44% due to continued injection drug use. Treatment with medication for opioid use disorder (MOUD) such as methadone, buprenorphine or naltrexone can decrease the likelihood of continued injection drug use and reinfection. The treatment episode for endocarditis offers an opportunity to initiate MOUD prior to discharge to reduce the likelihood of reinfection and overdose.
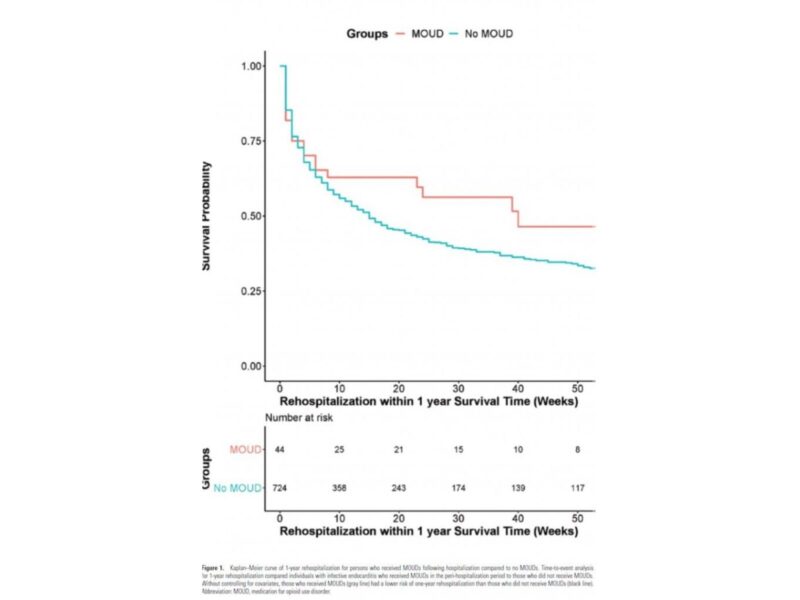
A recent study by CHERISH Research Affiliate Joshua Barocas, MD and colleagues at Boston Medical Center, Boston University, and Tufts Medical Center examined the rates of MOUD initiation among PWID following endocarditis treatment, and compared overdose and health outcomes among those who initiated MOUD and those who did not. This study examined treatment and health outcomes for 768 adults 18 years or older with opioid use disorder (OUD) who underwent endocarditis treatment between 2010- 2016 in the Marketscan commercial claims and encounters database. The study found that only approximately 6% of the individuals treated for endocarditis (44/768) initiated MOUD during the peri-hospitalization period or within 30 days of the index endocarditis hospitalization. Those who initiated MOUD were significantly younger than those who did not (average age of 25 and 40 years, respectively) and experienced fewer overdoses compared to those who did not (5.8 per 100 person years [PY] and 7.3 per 100 PY, respectively). They also experienced fewer episodes of opioid related re-hospitalizations during the one-year follow up (162.0 per 100 PY and 255.4 per 100 PY, respectively). In adjusted Cox proportional hazard models, however, the receipt of MOUD was not associated with either outcome. This may be attributed to low overall event occurrences or the lack of methadone treatment information in the claims database. Methadone was not reliably included in the data set and was not included in the analysis, because it was not covered by commercial insurance until late 2017. The study highlights a missed opportunity to engage PWID with endocarditis in MOUD care in order to reduce the risk of overdose, improve health outcomes, and reduce costly re-hospitalizations.
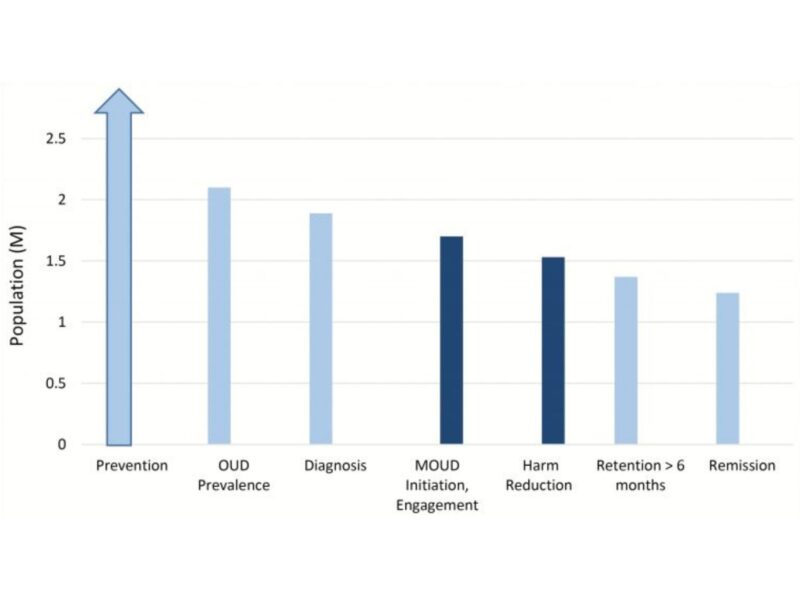
Dr. Barocas and colleagues conclude that there is a crucial need to improve low barrier access to MOUD, and early initiation of MOUD should be the standard of care for persons with OUD-related infections. An invited commentary by Ellen Eaton, MD, MSPH at the University of Alabama contextualizes these findings within the U.S. treatment system and insurance reimbursement structure. Dr. Eaton compares the financial support for the continuum of OUD care to that of HIV to illustrate how government funding influences treatment uptake and availability. People with OUD face several financial and physical barriers to accessing MOUD, such as waiting lists for treatment that are upwards of one year long and the low number of waivered physicians that is not distributed across the country in a pattern consistent with the greatest need. In contrast, people living with HIV can be initiated on ART on the day of diagnosis and connected to additional services due to continued government support through Ryan White funding and other avenues. In order to implement same day MOUD to improve long term health outcomes and address the opioid overdose epidemic, Dr. Eaton emphasizes the need for comprehensive funding and support for MOUD.