Association between claims-based setting of diagnosis and treatment initiation among Medicare patients with Hepatitis C
New study develops the first algorithm that utilizes claims data to assess the relationship between diagnosis settings and HCV treatment initiation.
Direct-acting antivirals (DAAs) have been available since 2015 for hepatitis C (HCV). Nonetheless, very few patients with HCV initiate DAA treatment, ranging from 5% to 30%. The location where a patient is first diagnosed can also influence the care patients receive afterward, especially when a referral to a specialist or coordinated care is needed. In this new study, lead author and former CHERISH pilot grantee Hao Zhang, CHERISH investigator Yuhua Bao, CHERISH Research Affiliate Shashi Kapadia, and Weill Cornell Medicine colleagues Kayla Hutchings and Martin F. Shapiro investigated this association for HCV treatment initiations using Medicare healthcare claims data.

Hao Zhang
Lead author and former CHERISH pilot grantee
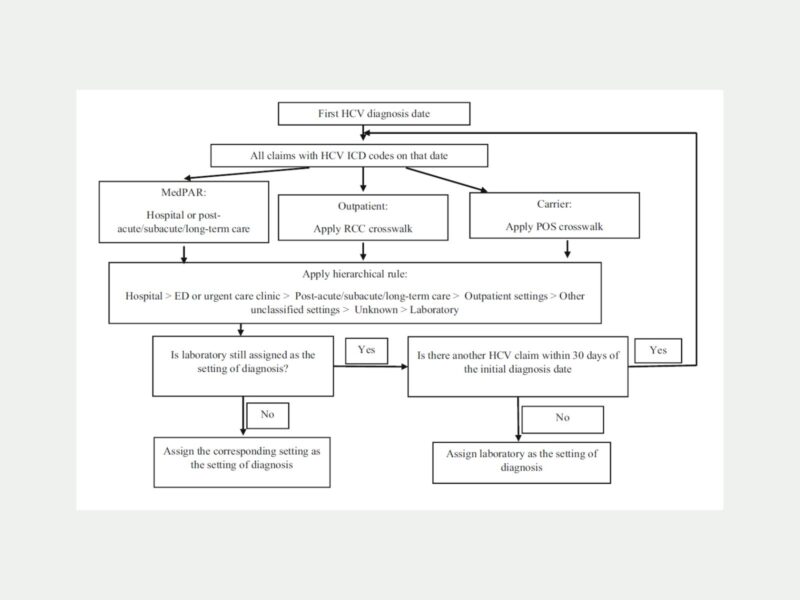
The team of researchers devised an algorithm to analyze a study sample of Medicare patients diagnosed with HCV between 2015 and 2019. The algorithm assigned a single diagnostic setting based on seven broad categories, hospital, emergency department (ED)/urgent care, outpatient, post-acute/subacute/long-term care, laboratory, unknown clinical settings, and other unclassified settings to each diagnosis. The details of the process the algorithm follows are shown in the figure above. Initiation of DAA treatment was defined as at least one DAA prescription within 180 days of the HCV diagnosis.
Key Findings
- The largest percentage of patients was diagnosed in outpatient clinics. The second largest percentage of patients was diagnosed in either laboratories or unknown clinical settings, followed by hospitals, other unclassified settings, and ED/urgent care.
- The patients diagnosed in hospitals or ED/urgent care settings were more likely to also have many comorbidities, including opioid use disorder, alcohol use disorder, advanced liver disease, HIV, and mental health disorder. In addition, these patients were less likely to be non-Hispanic White.
- The HCV treatment initiation rate was the highest for patients diagnosed in outpatient settings compared to patients diagnosed in EDs/urgent care, hospitals, laboratories, and other unknown settings.
Medicare patients diagnosed with HCV in outpatient clinics were more likely to initiate treatment for HCV compared to patients diagnosed in other clinical settings.
This health services study is the first of its kind to utilize a claims-based algorithm to assess the relationship between a diagnostic setting and HCV treatment initiation. The innovative algorithm can be applied to other health conditions where stigma or coordinated care impacts treatment initiation. The findings also indicated that the DAA initiation rate is lower in patients diagnosed in hospitals and ED/urgent care facilities than in patients diagnosed in outpatient clinics, providing greater insight into disparities in HCV treatment initiation and access to care. In addition, the analysis of claims data found that patients who were diagnosed in hospitals or ED/urgent care settings were more likely to have comorbidities, including opioid use disorder, alcohol use disorder, and HIV. To address this issue, authors suggest greater efforts to link patients to comprehensive care after diagnosis.
Read the full study published in Health Services Research.
Elsie Wong was a communications intern within the Division of Comparative Effectiveness and Outcomes Research of the Department of Population Health Sciences at Weill Cornell Medicine who assisted with promoting new research published by the Center for Health Economics of Treatment Interventions for Substance Use Disorders, HCV, and HIV. With her background in medicine and communications, Elsie aspires to become a physician to improve health literacy among underserved communities.