Racial and Ethnic Disparities Along the Hepatitis C Care Cascade Among Priority Populations
Studies highlight disparities in hepatitis C testing among reproductive-age females with opioid use disorder and children who were perinatally exposed to hepatitis C virus.

Over the last two decades, injection opioid use has increased among reproductive-aged women, with resultant increases in mother-to-child hepatitis C virus (HCV) transmissions in the U.S. Direct-acting antiviral (DAA) treatment is highly effective at reducing and eliminating the risk of HCV transmissions. Yet, studies show lower odds of receiving DAA treatment for women compared to men, and for Black non-Hispanic and Hispanic individuals compared to white individuals.
Despite the increasing HCV prevalence among pregnant people, HCV testing rates in their exposed children remain low. In response, the Center for Disease Control and Prevention (CDC) issued new guidelines in 2023 that now recommend testing exposed infants as early as 2 months of age with ribonucleic acid (RNA) testing as opposed to waiting until 18 months of age to complete antibody testing as previous guidelines recommended.
Early screening and testing for HCV remain essential in the national effort to eliminate HCV and prevent serious liver complications. Two new publications featuring CHERISH Research Affiliate Rachel Epstein, CHERISH pilot grantees Megan R. Curtis and Breanne Biondi, and Syndemics Lab colleague Sarah Munroe aim to inform HCV testing and treatment implementation strategies among priority populations while highlighting racial and ethnic disparities along the HCV care cascade.
Reproductive-age females with opioid use disorder
In a study published in Clinical Infectious Diseases, lead author and CHERISH pilot grant recipient Breanne Biondi, examined racial and ethnic disparities along the HCV care cascade among a national cohort of women with opioid use disorder (OUD).

Breanne Biondi, MPH
2024-2025 CHERISH pilot grant recipient
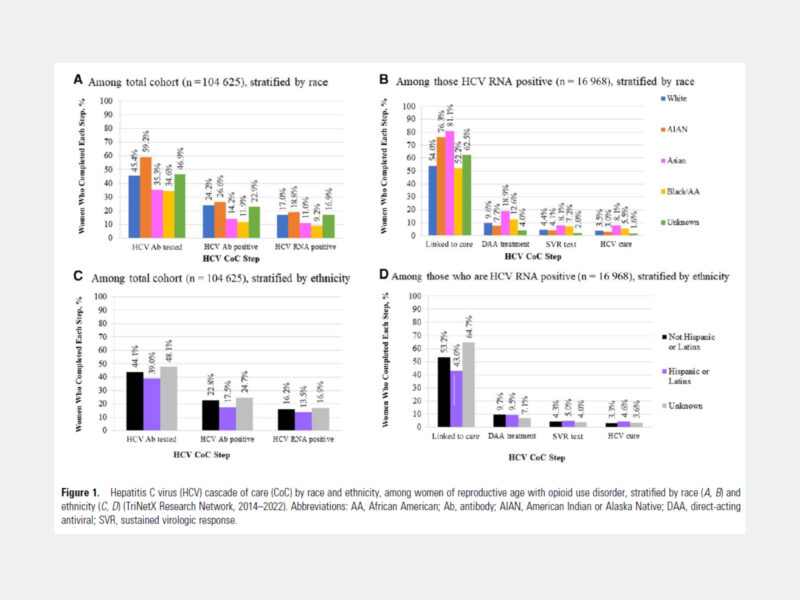
Biondi and co-authors used TriNetX, a real-time national electronic medical record database, to identify a cohort of more than 104,600 reproductive-age women, ages 15 to 44, who had any diagnosis of OUD from January 2014 to November 2022. Shown in the following figure, the HCV cascade included seven stages of care and was stratified by the race and ethnicity categories American Indian or Alaska Native (AIAN), Asian, Black/African American, White, Hispanic/Latinx, non-Hispanic/Latinx, and unknown.
Key Findings
- Less than half of the cohort received HCV antibody testing and nearly a quarter of the cohort had a positive HCV antibody test.
- Asian and Black/African American women were 25% less likely to have an HCV antibody test compared to white women.
- Hispanic/Latinx women, compared to non-Hispanic/Latinx women, were more likely to start DAA treatment when linked to care.
- Regionally, the West had the highest likelihood of HCV antibody testing. The South had the lowest likelihood of HCV antibody testing, particularly for AIAN, Asian, Black/African American, and Hispanic/Latinx women.
Less than 10% of women with OUD and HCV infection received treatment. To reduce the risk of perinatal HCV transmissions among this population, care strategies must address barriers to healthcare among women of color.
Findings from this study not only demonstrated poor HCV testing rates among reproductive-aged women but also highlighted differences in the stages of care across racial and ethnic groups. The authors call for targeted efforts to improve HCV testing and treatment for women with OUD, particularly among minoritized populations in select U.S. regions. Evidence-based strategies, such as offering medications for OUD alongside HCV treatment, and integrating low-barrier, non-stigmatizing, and culturally sensitive care are crucial to building equitable care and reducing the HCV burden among women from minoritized communities. Furthermore, HCV care models for reproductive-aged women must continue to innovate and be evaluated to achieve higher rates of HCV screening and treatment.
Infants who were perinatally exposed to hepatitis C
In a second study, published in the Journal of the Pediatric Infectious Diseases Society, lead author and CHERISH Research Affiliate Rachel Epstein, led a retrospective study to describe the HCV care cascade in the U.S. among children perinatally exposed to HCV.

Rachel Epstein, MD, MSc
CHERISH Research Affiliate
Epstein and co-authors used TriNetX to identify a cohort that included infants born between 2010-2020 with exposure to HCV. They extracted data on more than 8,500 infants to characterize the HCV care cascade by age, race, ethnicity, region, and treatment outcomes. The HCV care cascade, shown in the following figure, depicts key outcomes for HCV-exposed infants, from HCV testing to diagnosis of HCV infection, and then for those eligible for treatment, evidence of linkage to care and treatment.
Key Findings
- Less than half of HCV-exposed children completed appropriate testing for HCV.
- Only 1 in every 7 children who were eligible for treatment were treated.
- Black, Asian/Pacific Islander, and Hispanic/Latinx children had lower odds of testing for HCV.
- There were higher odds of HCV RNA testing in the Midwest (compared to Northeast), among Black children (compared to white children), and among children born between 2018-2020 (compared to children born between 2010-2013).
In a national sample of HCV-exposed infants, more than half did not have evidence of completing any HCV testing. Testing early and addressing racial, ethnic, and regional disparities may help improve treatment outcomes.
The HCV care cascade captured in this study points to a lack of testing and treatment for HCV-exposed infants, particularly for Black, Asian/Pacific Islander, and Hispanic/Latinx children. The racial, ethnic, and regional disparities observed in the study likely reflect various socioeconomic and environmental barriers to care, including disruptions from the COVID-19 pandemic. To reach national HCV elimination goals, the authors call for improvements in HCV testing and treatment for racial and ethnic minority populations, for patient and provider education, and for better understanding of systemic biases within healthcare and how to dismantle them. Future research directions can also explore integrated models of maternal-infant care to improve the HCV care cascade for vulnerable populations.
“Racial and ethnic disparities in testing of Hepatitis C virus-exposed children across the United States,” was published on August 22, 2024, in the Journal of the Pediatric Infectious Diseases Society and supported, in part, by a CHERISH pilot grant awarded to Megan Rose Curtis in 2022.
“Racial and Ethnic Disparities in Hepatitis C Care in Reproductive-Aged Women With Opioid Use Disorder,” was published on October 2, 2024, in Clinical Infectious Diseases. This article has also been featured in Healio on November 5, 2024, in an interview with Rachel Epstein and Bre Biondi.