Two New Publications Address Expanding Access to HCV Care Among People Who Inject Drugs
Hepatitis C Virus (HCV) is one of the leading causes of infectious disease deaths in the United States. Injection drug use is a common route of HCV transmission and the annual number of reported cases continues to rise due to the opioid epidemic. Previous HCV treatment regimens had severe side effects and limited efficacy, but current direct-acting antivirals (DAAs) have made HCV almost universally curable. Due to the initial high cost of DAAs, many state Medicaid programs had strict eligibility criteria to access treatment, such as requiring evidence of abstinence from substance use. Many programs have recently relaxed these restrictions.
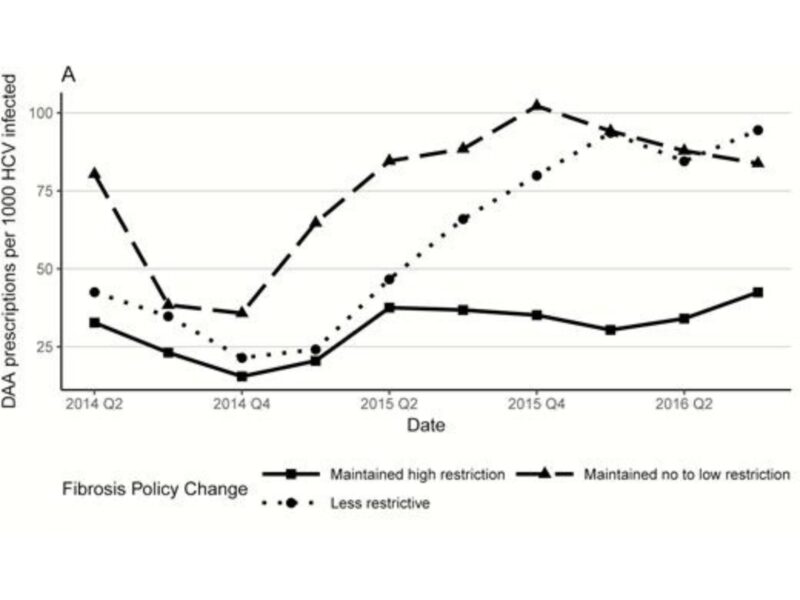
In a recent publication in Clinical Infectious Diseases, CHERISH trainee Dr. Shashi Kapadia, CHERISH staff member Philip Jeng, CHERISH director Dr. Bruce Schackman and CHERISH research affiliate Dr. Yuhua Bao characterize variation in DAA utilization among states and explore the association between changes in Medicaid treatment eligibility criteria and trends in DAA utilization. Their analysis finds that those states that relaxed Medicaid DAA treatment eligibility requirements in terms of disease severity and substance use abstinence had larger increases in treatment utilization for HCV-infected Medicaid enrollees from 2014 to 2016. They also found an increase in DAA utilization in states that implemented Medicaid expansion under the Affordable Care Act.
Although removing eligibility criteria can increase treatment access for individuals who are identified and linked to care, barriers to HCV screening and linkage persist for people who inject drugs. Dr. Schackman, along with CHERISH investigators Sarah Gutkind, Dr. Jake Morgan, Jared Leff, Dr. Czarina Behrends and Dr. Benjamin Linas examined the cost-effectiveness of screening and linkage to care models for patients in methadone maintenance treatment (MMT) programs in New York and San Francisco. Using data from a published clinical trial, they compared hepatitis screening and education only to an intervention that added HCV care coordination and linkage. They used a computer simulation model that evaluated lifetime costs and benefits, and concluded that HCV screening and education with care coordination in MMT programs presents an efficient use of resources.
This article was published in Drug and Alcohol Dependence and is available for download online without charge for the next 6 months.