Targeting Emergency Department Resources to Address the Opioid Epidemic
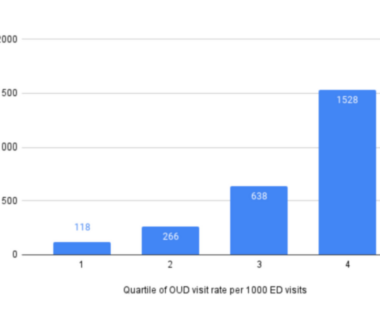
In a new study in the American Journal of Emergency Medicine, my colleagues and I estimate the number and distribution of emergency visits for opioid use disorder (OUD) across the country. We found that nearly 2/3 of all emergency visits for OUD occurred in 25% of EDs nationwide. Why is this important? Patients with OUD come to the […]

The Impact of Recreational Cannabis Laws and Cannabis Use Disorder Among Pregnant Patients
To date, the American College of Obstetricians and Gynecologists advises pregnant patients not to use cannabis because of the increased risks of health complications to the pregnant individual and the newborn. However, as states expand access to recreational or medical cannabis, there is growing evidence of increased cannabis use and positive perceptions of cannabis among pregnant patients. […]

Robust Prescription Monitoring Programs and Abrupt Discontinuation of Long-term Opioid Use
Prescription drug monitoring programs (PDMPs) are statewide databases that track controlled substances dispensed at retail pharmacies. Used by health care providers, public health officials, and other stakeholders, PDMPs have become a major tool in addressing unsafe opioid prescriptions. Robust features of PDMPs—including mandates that allow prescriber use of PDMP, data-sharing across states, and prescriber delegation of […]
Prescription Opioids Dispensed to Patients with Cancer with Bone Metastasis: 2011-2017
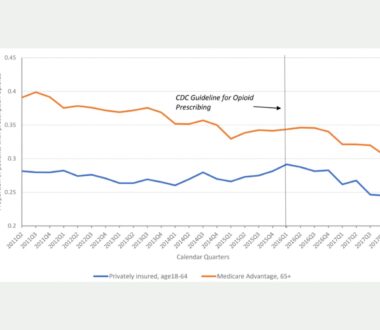
In the past decade, opioid prescribing in the United States has steadily decreased as federal and state officials implemented strict regulations on prescription opioids to address the opioid crisis. The downward trend sparked concerns of undertreating chronic pain and prompted the Centers for Disease Control and Prevention (CDC) to formally clarify that the 2016 CDC […]

Hepatitis C Treatment by Non-specialist Providers in the Direct-acting Antiviral Era
Direct-acting antiviral agents (DAAs), highly effective treatments for hepatitis C virus infection (HCV), transformed HCV therapy and made it easier for non-specialist providers to prescribe HCV treatment. Despite this simplification, many insurers include being a specialist as part of prior authorization requirements for DAA treatment. CHERISH Research Affiliate and former pilot grant recipient Shashi N. […]

Prescription Drug Monitoring Program Mandates Affect Use of Opioids to Treat Acute, Severe Pain
Prescription drug monitoring programs (PDMP) have been crucial tools to address unsafe opioid prescribing. High rates of prescribing stoked the flames of the opioid crisis in the early 2000s, but opioid prescriptions have steadily decreased over the past decade. Unfortunately, opioid-related deaths have continued to rise each year. Many states have enacted comprehensive mandates that all clinicians consult the PDMP […]

Characterizing Initiation, Use, and Discontinuation of Extended-Release Buprenorphine in a Nationally Representative United States Commercially Insured Cohort
Medications for opioid use disorder (MOUD) are evidence-based treatments that help people reduce or stop using opioids. However, high discontinuation rates of MOUD pose a barrier to reducing opioid-related overdoses. Extended-release buprenorphine (XR-BUP) is a relatively new MOUD, approved in late 2017, that has the potential to increase retention because of its monthly dosing schedule. Currently, there is […]
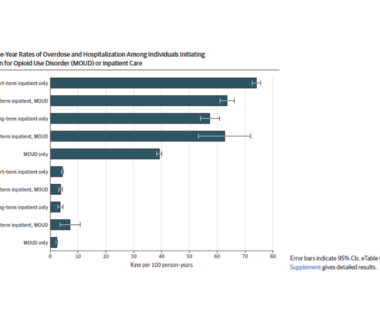
Inpatient care versus outpatient MOUD treatment for individuals with OUD
In a new study in JAMA Network Open, CHERISH investigators Jake Morgan, Sean Murphy, Alexander Walley, Benjamin Linas and Bruce Schackman and colleagues, examined whether rates of opioid-related overdose and all-cause hospitalization differed after outpatient medication treatment or inpatient care for opioid use disorder. They studied individuals who had received one of three federally- approved medications […]

Patients Get More Opioids Than They Need After Knee Arthroscopy
In our new study in BMJ Open, we show that in 2015-2019 more than 70% of U.S. opioid-naive patients received an opioid prescription after knee arthroscopy. They received an average of 40 tablets, despite recent studies showing most patients end up taking less than 5 tablets. The take-home message? Despite recent attention to opioid stewardship, we find wide variation […]
After Opioid Overdose Emergency, Few Patients Receive Timely Follow-up
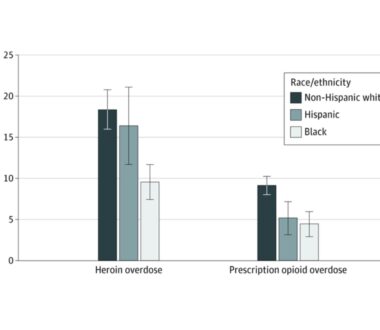
An opioid overdose is significantly more than an isolated event. Patients who present to the emergency department (ED) with overdose have a 6 percent risk of dying in the following year. As with other high-risk acute conditions, we expect patients who survive overdose to receive evidence-based treatment after leaving the hospital. Whether the overdose was due to prescription […]

Overdose and Re-hospitalization Rates Following Endocarditis Are Lower for Patients Receiving Medications for Opioid Use Disorder
The proportion of hospital admissions for endocarditis attributable to injection drug use increased from 7% in 2000 to 12% in 2013. Endocarditis is an infection in the lining of the heart chambers and valves that can be contracted through shared injection equipment. Rates of endocarditis are disproportionately affecting young people who inject drugs (PWID), which has […]

Will Eliminating Waiver Requirements Improve Access to Buprenorphine for Treating Opioid Use Disorder? Evidence From Increasing the Patient Treatment Cap
The Drug Addiction Treatment Act of 2000 (DATA 2000) permits qualified physicians to obtain a waiver to treat patients with opioid use disorder (OUD) with buprenorphine in office-based practices. In 2016, 47% of all US counties and 72% of rural counties lacked a buprenorphine waivered physician. That year, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing […]
Engage with CHERISH
Submit a Consultation Request or Contact Us to learn more about how CHERISH can support your research or policy goals.